Indwelling Pleural Catheter
This leaflet explains about having fluid drained from your chest using an indwelling pleural catheter. It will help you to understand the treatment, procedure and the care that you will receive.
If you would like additional information about an indwelling pleural catheter and what is involved, please speak to one of the doctors or nurses. They will be more than happy to help.
What is an indwelling pleural catheter? (IPC)
An indwelling pleural catheter (IPC) is a soft, flexible tube or drain that is used to remove fluid from your lung. One end of the tube remains in the chest while the rest passes through the skin. There is a one-way valve which prevents any fluid leaking out or air entering in. When the fluid builds up, the IPC can be used to drain excess fluid from your lungs. This is done by the district nurse using a pre-vacuumed bottle which attaches to the tube on the surface of your chest.
Why do I need one?
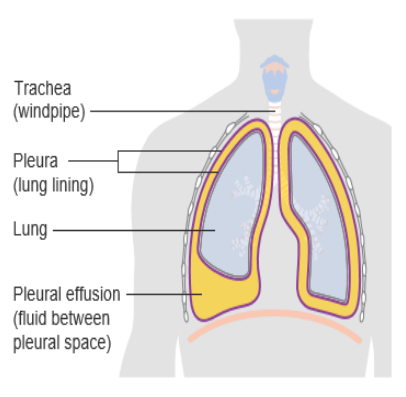
The fluid which has built up is between the ribcage and the lung. This is called the pleural cavity, or space, and there are two thin linings. There is normally a small amount of fluid between these two linings which allows the lungs to move when you breathe in an out.
In your case there is a larger amount of fluid in this space which causes increasing discomfort and shortness of breath. We can see this on a chest x-ray. The build-up of fluid can make it difficult for your lungs to expand. Draining this fluid will relieve your breathlessness. However, this fluid often builds up again. By using an IPC that can remain in place, this allows the fluid to be drained repeatedly without having to come into hospital each time the procedure needs doing.
There are many reasons the fluid can build in your lungs and some include, infection, heart problems and sometimes cancer. This will be discussed with you by the doctor when you attend the clinic.
What is involved?
You will be asked to attend pleural clinic. It is important that we know in advance if you are on any blood-thinning medication (anticoagulants), as they may need to be temporarily stopped prior to the procedure.
You will be asked for your consent and will then lie in a comfortable position. Your chest will be cleaned with antiseptic. Local anaesthetic is injected into your skin which initially stings, but will then numb the area to make it more comfortable. An ultrasound is used so that the doctor can see the amount of fluid and what it looks like. The Doctor then makes two cuts.
One cut is to put the tube into your chest and the second is to pass it through your skin. The IPC is then eased into your chest. Some of the fluid that is drained may be sent to the laboratory for testing.
Is there an alternative treatment?
We can insert a chest drain. This requires admission to hospital. Once all the fluid is drained, we can undertake a ‘Pleurodesis.’ This involves inserting medical talc into the chest drain to help stick the pleural spaces together and prevent the pleural fluid from re-accumulating.
We can perform a therapeutic pleural aspiration. We insert a small tube into the pleural space, drain off up to one litre of fluid, and then remove the tube. If the fluid re-accumulates, this procedure can be repeated.
The doctor will explain these options to you.
Care of your IPC
The catheter is covered with a clean, flat dressing which will enable you to shower or bathe and continue normal exercise. You will NOT be able to swim. There will be two sets of stitches. The first set (furthest from the drain) can be removed in seven to 10 days, while the second set can be removed 14 days later. This will be done by the district nurse. The IPC stays in place after this, as there is a soft cuff inside which your
skin will heal around making it secure.
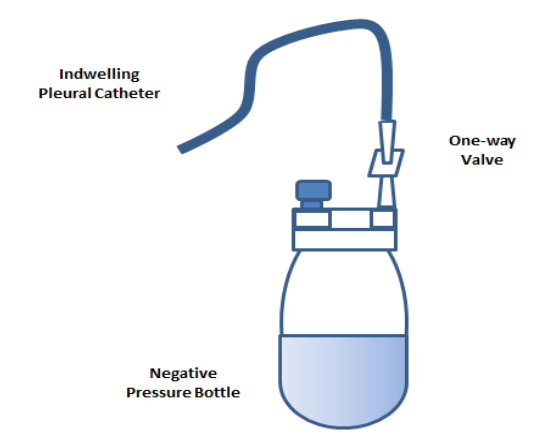
The district nurse will then use bottle and dressing kits each time to drain your lung. We currently use ‘rocket’ drains (see picture) and the district nurse will be able to order these for you. It is a good idea to have a spare one at home in case you are brought into hospital, as they are not part of routine stock.
Drainage can be done as regularly as needed initially, often on Monday, Wednesday and Friday, but this can be reduced as the amount of fluid decreases. Keeping a record of the volume of each drainage is advised. No more than 500mls should be drained at any one time. If drainage volume is less than 50mls on three consecutive occasions, the district nurse can speak to the nurse specialists/respiratory consultants
Are there any risks?
In most cases this is a safe, routine procedure. However, with all medical procedures there are risks:
- You may notice some discomfort for up to a week and you may take pain-killing tablets. The district nurse can also drain your fluid more slowly if pain/breathlessness or a cough occurs during drainage
- Infection is uncommon. If you develop a high temperature, or notice increasing pain or redness around the drain, contact the district nurse. Good catheter care will help to minimise this
- There is the rare risk of bleeding, as the drain may accidentally damage a blood vessel
- If the drain suddenly stops draining, and you remain short of breath, this may be due to a blockage. The IPC can be flushed to clear this.
Contact numbers
We hope that you have found this information useful. If you have any questions, or are worried about anything, please speak to the following Dorset County Hospital staff:
Respiratory consultants: 01305 255259
Nurse specialists: 01305 255289
Useful websites
My Pleural Effusion Journey: https://mypleuraleffusionjourney.com/
Macmillan: www.macmillan.org.uk/cancer-information-and-support/impacts-of-cancer/pleural-effusion
About this leaflet
Author: Erica Mason, Associate Specialist Nurse, Respiratory
Written: November 2020
Approved: January 2021
Review date: January 2024
Edition: v1
If you have feedback regarding the accuracy of the information contained in this leaflet, or if you would like a list of references used to develop this leaflet, please email patientinformation.leaflets@dchft.nhs.uk
Print leaflet