What is Quality Improvement?
Quality improvement (QI) provides a framework to look at what we do and to see if we could do it better. It is looking at things big or small with a different lens.
QI uses a systematic evidence-based approach and uses tools and techniques to improve the experience and the outcomes for colleagues, service users and their families and carers. It can also be used to improve our working environment, for example, improve our own processes to free up time to care.
QI utilises the subject matter expertise of people closest to the issue including staff and service users to identify potential solutions and test them.
It allows everyone to have a voice and feel empowered to take part in making a real difference.
Click here for a step-by-step QI guide.
Why does quality improvement matter?
Every health care system is built on a complex network of care processes and pathways. The quality of the care delivered by the system depends to a large extent on how well this network functions, and how well the people who provide and manage care work together.
The overall aim is simple: to provide high-quality care to patients and improve the health of our population. Yet, as every patient and professional can testify, for every process or pathway that works well, there is another that causes delay, wasted effort, frustration or even harm.
Quality improvement is about giving the people closest to issues affecting care quality the time, permission, skills and resources they need to solve them. It involves a systematic and coordinated approach to solving a problem using specific methods and tools with the aim of bringing about a measurable improvement.
Done well, quality improvement can deliver sustained improvements not only in the quality, experience, productivity and outcomes of care, but also in the lives of the people working in health care. For example, it can be used to improve patient access to their GP, streamline the management of hospital outpatient clinics, reduce falls in care homes, or tackle variations between providers in the way processes and activities are delivered.
An understanding of quality improvement is therefore important for anyone who delivers or manages care, as well as for people using care services and wondering how they could be improved. Through quality improvement there is the potential to create a health care service capable of ensuring ‘no needless deaths; no needless pain or suffering; no helplessness in those served or serving; no unwanted waiting; no waste; and no one left out.
Why does quality improvement matter to Dorset?
As an ICS we are developing a culture of continuous improvement. QI builds on foundations we already had in place and work we were already doing across the system but is a more proactive approach and brings various tried and tested methodologies altogether in one place.
Our health trusts regulator, the Care Quality Commission (CQC), recommends the QI approach and 80% of trusts who have fully embedded QI are rated as outstanding. NHS trusts across the country are using QI to make changes which will lead to better patient outcomes, better care, an improved service, efficiencies and an improved working environment for colleagues.
Quality improvement training
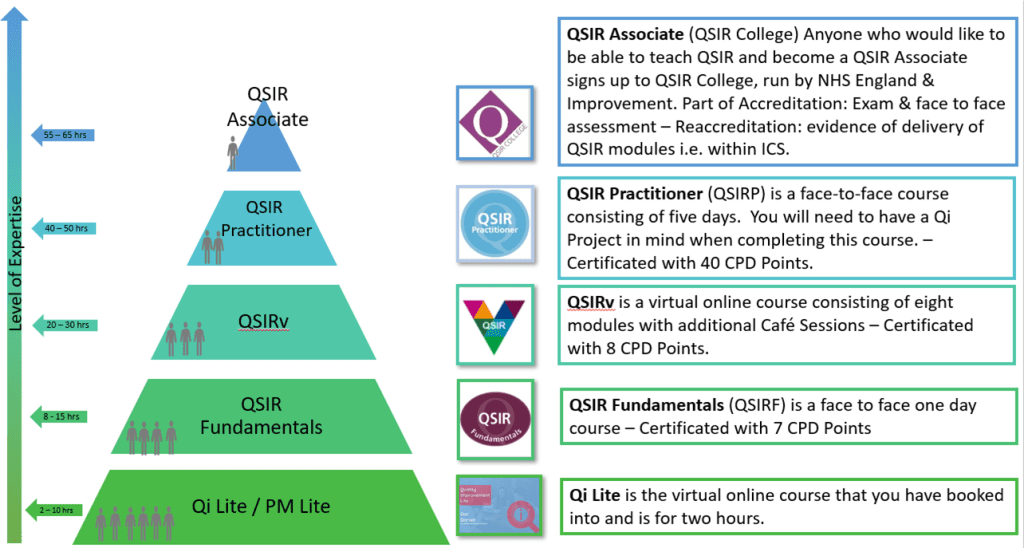
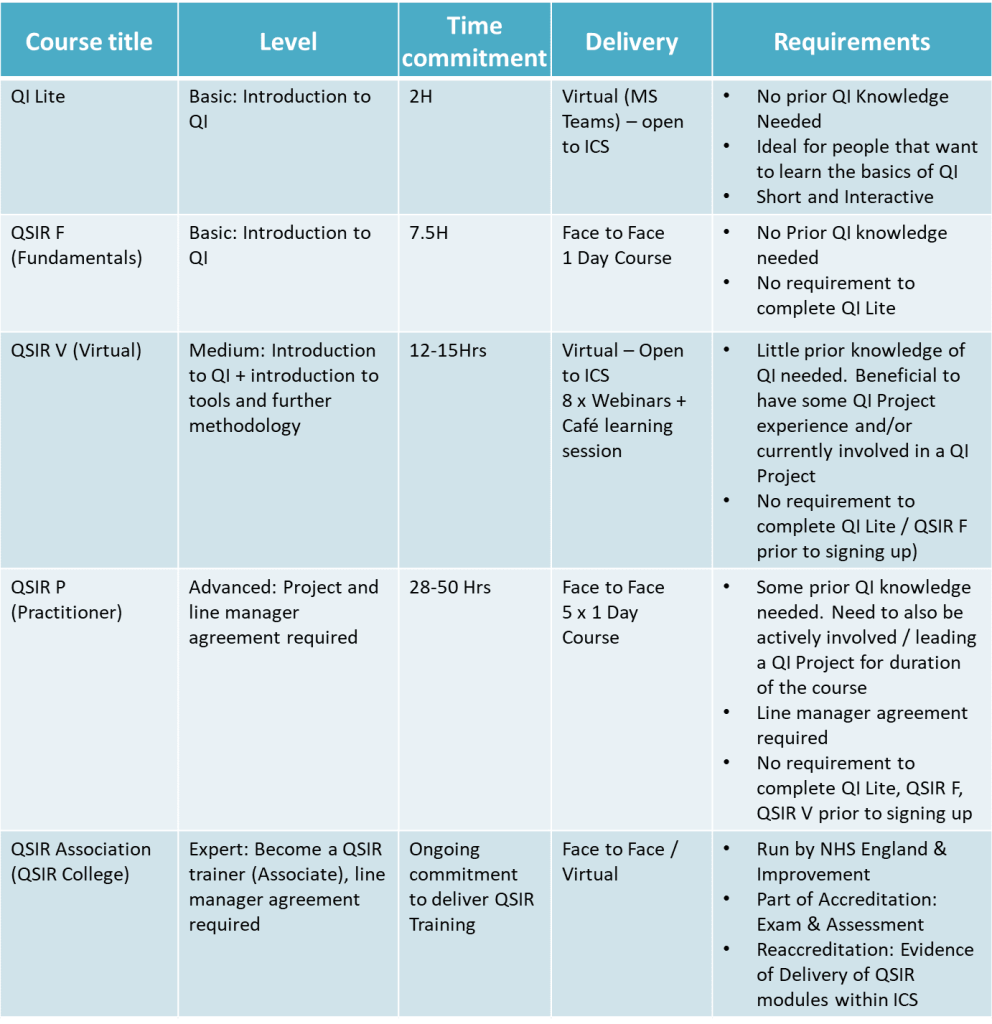
We have a variety of training offers across Dorset. QI training is available to all staff across the Integrated Care System of Dorset and is offered in a tiered approach dependant on your existing knowledge and experience.
The training levels are as follows:
- QI Lite an Introduction to Quality Improvement
- QSIR Fundamentals and QSIR Virtual
- QSIR Practitioner
- QSIR Associate Member
If you would like to register for one of the upcoming QI Lite training sessions, please email transformationoffice@dchft.nhs.uk.
If you would like to register for an upcoming QSIR Pracitioner course, please email transformationoffice@dchft.nhs.uk.
Contact us
If you would like to get in touch with the team, please email transformationoffice@dchft.nhs.uk
